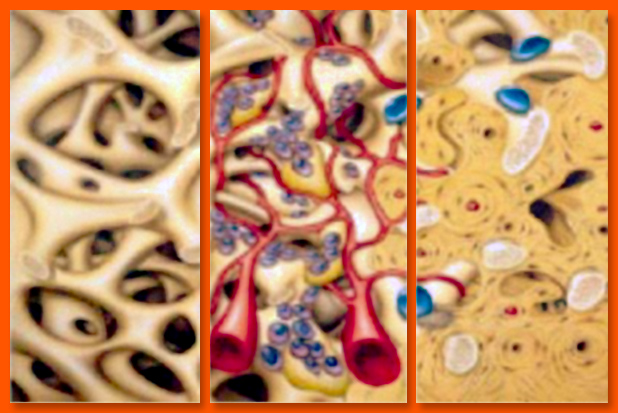
Guided bone regeneration emerged from periodontology and the Guided Tissue Regeneration (GTR) technique. Described by Nyman et al. in 1980 and 1982, the biological procedure for GTR uses a physical barrier enabling cellular recolonisation of radicular surfaces by periodontal cells(1),(2),(3).
This idea was broadened to include bone regeneration by Dahlin et al. in 1988, inspired by the findings of Murray et al. in 1957, who had noted bone regeneration within a plastic cage introduced to a bone defect in the iliac bone of a dog(4), they discovered it was possible to reform bone around implants placed in rabbit tibias and covered with ePTFE (expanded polytetrafluoroethylene) membranes(5).
The first GBR used a rigid membrane for blood clot stabilisation and for ensuring osteogenic cells were able to colonise and regenerate the space, in this way protected from invasion, with junctional epithelium cells which heal more rapidly.
Biomaterials were then added enabling support of the membrane, which was no longer required to be rigid, to leave space for less restrictive resorbable membranes. Next, variants appeared, such as use of osteosynthesis screws to maintain the membrane at a distance such as “tent poles” or use of cortical bone slices as rigid membranes in formwork techniques.